Peripheral Blood Stem Cell Transplant
Peripheral Blood Stem Cell Transplant (PBSCT), also known as a peripheral blood stem cell infusion, is a medical procedure that has revolutionized the treatment of various life-threatening diseases, particularly those related to the blood and immune system. This advanced therapeutic approach involves the transplantation of stem cells from the peripheral blood, offering new hope to patients facing conditions such as leukemia, lymphoma, and certain genetic disorders.
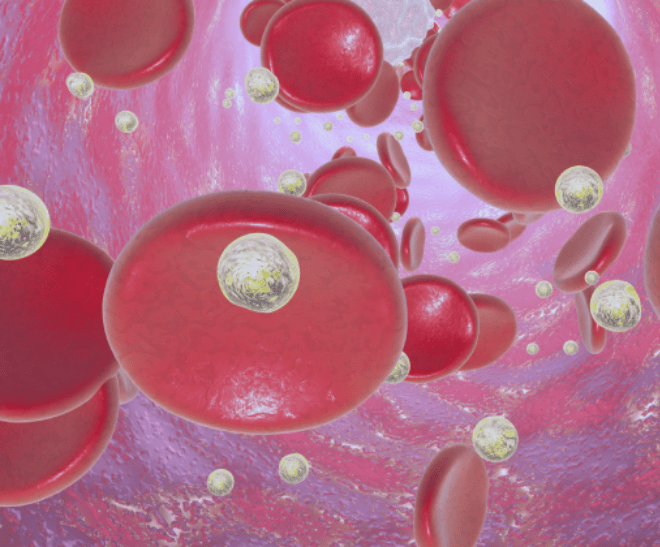
Peripheral Blood Stem Cells (PBSCs) are a type of multipotent stem cell found in the bloodstream. These cells have the remarkable ability to differentiate into different types of blood cells, including red blood cells, white blood cells, and platelets. In PBSCT, these cells are harvested from the donor’s blood and play a crucial role in rebuilding the patient’s damaged or depleted blood and immune system.
Mobilization:
- Before the harvest, donors may undergo a process called mobilization, where growth factors are administered to stimulate the release of stem cells from the bone marrow into the bloodstream.
- This step ensures a sufficient number of stem cells are present in the peripheral blood for collection.
Collection:
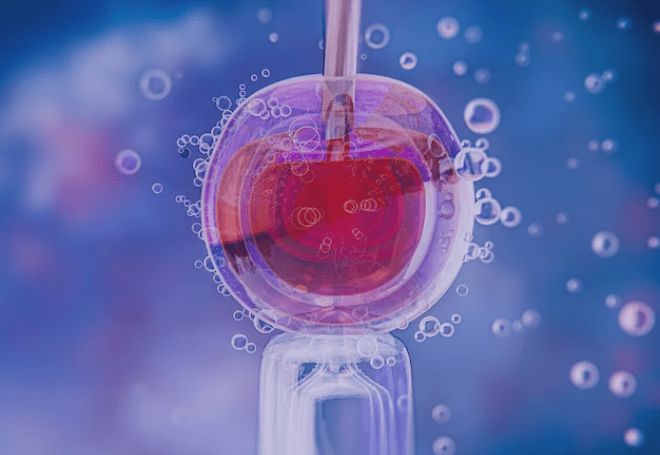
- The actual collection of stem cells is performed through a process called apheresis. During apheresis, blood is drawn from the donor, and a machine separates the stem cells from other blood components.
- The remaining blood components are returned to the donor, making the process non-invasive and generally well-tolerated.
Processing and Storage:
- The collected stem cells undergo processing to remove any remaining contaminants. Once purified, these cells are cryopreserved for future use.
- Cryopreservation allows for long-term storage, ensuring the viability of the stem cells until they are needed for transplantation.
Transplantation:
- The patient undergoing transplantation receives high-dose chemotherapy and/or radiation to destroy diseased or malfunctioning cells in the bone marrow.
- The cryopreserved peripheral blood stem cells are then thawed and infused into the patient’s bloodstream.
- Over time, these cells migrate to the bone marrow and begin the process of creating new, healthy blood and immune cells.
Reduced Recovery Time:
- Compared to traditional bone marrow transplants, PBSCT often results in a faster recovery, as the donor’s blood cells return to normal levels more rapidly.
Broader Donor Pool:
- PBSCT allows for a more diverse donor pool, as it is not limited to identical or closely matched siblings. This increases the likelihood of finding a suitable donor for patients in need.
Lower Risk of Graft-versus-Host Disease (GVHD):
- GVHD, a potential complication of transplantation, occurs when the donor’s immune cells attack the recipient’s tissues. PBSCT has been associated with a lower incidence of severe GVHD compared to bone marrow transplants.
Before Transplant (Preparative Phase):
- Fatigue: High-dose chemotherapy and/or radiation therapy can lead to fatigue.
- Nausea and Vomiting: Common side effects of chemotherapy.
During Transplant (Infusion Phase):
- Fever: Common during and after the stem cell infusion.
- Chills: Shivering or feeling cold may occur.
- Shortness of Breath: Some individuals may experience difficulty breathing.
After Transplant (Engraftment Phase):
- Low Blood Cell Counts:
- Anemia: Fatigue, weakness, and pale skin.
- Neutropenia: Increased risk of infections.
- Thrombocytopenia: Easy bruising, bleeding, and a low platelet count.
- Mucositis: Inflammation and sores in the mouth and gastrointestinal tract, leading to pain and difficulty eating.
- Graft-versus-Host Disease (GVHD): Symptoms may include skin rash, diarrhea, and liver problems.
Peripheral Blood Stem Cell Transplants have emerged as a transformative treatment option, offering renewed hope to individuals grappling with serious blood-related disorders. As medical advancements continue, the refinement of PBSCT techniques and the expansion of donor accessibility contribute to a brighter future for patients in need of life-saving interventions. The journey from donor mobilization to transplantation represents a remarkable collaboration between science, medicine, and the altruism of those willing to make a difference in the lives of others.
Autologous Bone Marrow Transplant
Autologous Bone Marrow Transplantation (ABMT), also known as autologous stem cell transplant, is a medical procedure that utilizes a patient’s own stem cells to treat certain conditions, particularly those involving the blood and immune system. This innovative approach represents a remarkable synergy between medical science and the body’s inherent regenerative capabilities, offering new avenues of hope for individuals facing diseases such as multiple myeloma, lymphoma, and certain types of leukemia.
Reduced Risk of Graft-versus-Host Disease (GVHD):
- Since the transplanted cells come from the patient’s own body, the risk of GVHD—a common complication in allogeneic transplants where the donor’s immune cells attack the recipient’s tissues—is significantly reduced.
Broader Applicability:
- Autologous transplants are not limited by the need for a perfectly matched donor. This makes the procedure accessible to a larger number of patients, as it relies on the individual’s unique biological material.
Lower Risk of Infection:
- Patients typically experience a shorter period of immune suppression compared to allogeneic transplants, resulting in a lower risk of infections during the recovery phase.
Faster Recovery Time:
- The recovery period for autologous transplants is often shorter compared to allogeneic transplants. Patients may experience a quicker return to normal blood cell counts and a reduced duration of hospitalization.
The procedure of Autologous Bone Marrow Transplant (ABMT) involves several key steps, from the harvesting of the patient’s own stem cells to the reinfusion of these cells following intensive chemotherapy or radiation therapy. Here is an overview of the typical procedure:
Evaluation and Pre-transplant Assessment:
- Before the transplant, the patient undergoes a comprehensive evaluation to assess their overall health and determine their eligibility for the procedure.
- Diagnostic tests, such as imaging studies and blood tests, are conducted to evaluate the extent of the disease and the general condition of the patient.
Stem Cell Harvesting:
- The patient’s own stem cells are collected before the transplant. This can be done through two main methods:
- Bone Marrow Harvesting: A minor surgical procedure where a needle is inserted into the hipbone to withdraw bone marrow containing stem cells.
- Peripheral Blood Stem Cell Collection (Apheresis): Blood is drawn from the patient, and a machine separates and collects the stem cells. This method is more common and less invasive than bone marrow harvesting.
Preparative (Conditioning) Regimen:
- Before the reinfusion of stem cells, the patient undergoes a preparative or conditioning regimen.
- This involves high-dose chemotherapy and sometimes radiation therapy to destroy cancer cells in the bone marrow and suppress the patient’s immune system, creating space for the new stem cells to engraft.
Stem Cell Infusion:
- Once the preparative regimen is completed, the harvested stem cells are infused back into the patient’s bloodstream. This process is similar to a blood transfusion.
- The stem cells circulate in the bloodstream and eventually migrate to the bone marrow, where they begin to produce new blood cells.
Before Transplant (Preparative Phase):
- Fatigue: High-dose chemotherapy used in the preparative phase can lead to significant fatigue.
- Nausea and Vomiting: Common side effects of the preparative chemotherapy.
During Transplant (Infusion Phase):
- Fever: Fever can occur during and after the infusion of autologous stem cells.
- Chills: Shivering or feeling cold may accompany the fever.
- Shortness of Breath: Some individuals may experience difficulty breathing.
After Transplant (Engraftment and Recovery Phase):
- Low Blood Cell Counts:
- Anemia: Fatigue, weakness, and pale skin.
- Neutropenia: Increased risk of infections.
- Thrombocytopenia: Easy bruising, bleeding, and a low platelet count.
- Mucositis: Inflammation and sores in the mouth and gastrointestinal tract, leading to pain and difficulty eating.
- Infections: Patients may remain at an increased risk of infections until the immune system fully recovers.
- Changes in Appetite and Taste: Some individuals may experience changes in taste or have a reduced appetite.
Recovery Phase:
- Fatigue: Lingering fatigue may persist as the body continues to recover.
- Skin and Nail Changes: Dry skin, rashes, and changes in nail texture may occur.
- Muscle and Joint Pain: Some patients may experience muscle and joint pain during recovery.
Autologous Bone Marrow Transplantation stands as a testament to the progress in medical science, offering a personalized and less complex approach to treating various hematological conditions. This innovative procedure not only leverages the regenerative potential of the body’s own cells but also extends the hope of recovery to a broader spectrum of patients. As research continues and technology evolves, the landscape of autologous transplants is likely to expand, providing even more effective and tailored solutions for individuals facing blood-related disorders.
Allogeneic Bone Marrow Transplant
Allogeneic Bone Marrow Transplant (allo-BMT) stands as a transformative medical procedure that harnesses the power of donor cells to treat a range of life-threatening conditions, particularly those affecting the blood and immune system. This advanced therapeutic approach involves the transfer of healthy bone marrow from a genetically matched donor to a recipient, offering a potential cure for diseases such as leukemia, lymphoma, and certain genetic disorders.
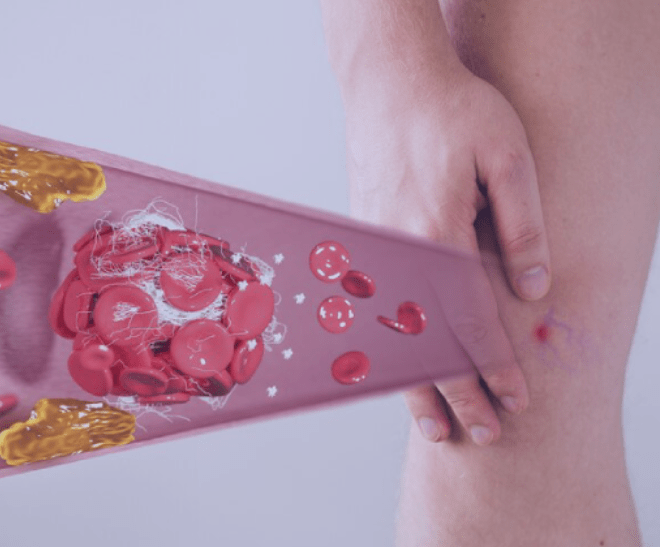
Graft-versus-Host Disease (GVHD):
- GVHD can occur when the donor’s immune cells attack the recipient’s tissues. Prophylactic measures and careful monitoring are implemented to manage and mitigate this potential complication.
Infection Risk:
- The recipient may experience an increased risk of infections, particularly during the initial phase of immune system recovery.
Donor Matching:
- Allo-BMT relies on finding a suitable donor whose tissue type closely matches that of the recipient. This is crucial to minimize the risk of graft-versus-host disease (GVHD) and improve the chances of successful engraftment.
Preparative (Conditioning) Regimen:
- Before the transplant, the recipient undergoes a preparative regimen, which involves high-dose chemotherapy and sometimes radiation therapy.
- This intensive treatment aims to eliminate diseased or malfunctioning cells in the recipient’s bone marrow, making room for the healthy donor cells.
Bone Marrow Harvesting from Donor:
- Donor bone marrow is typically harvested through a procedure called bone marrow aspiration. This involves the insertion of a needle into the donor’s hipbone to withdraw bone marrow containing hematopoietic stem cells (HSCs).
- Alternatively, peripheral blood stem cells may be collected from the donor through apheresis, a process where blood is drawn, and a machine separates and collects the stem cells.
Stem Cell Infusion:
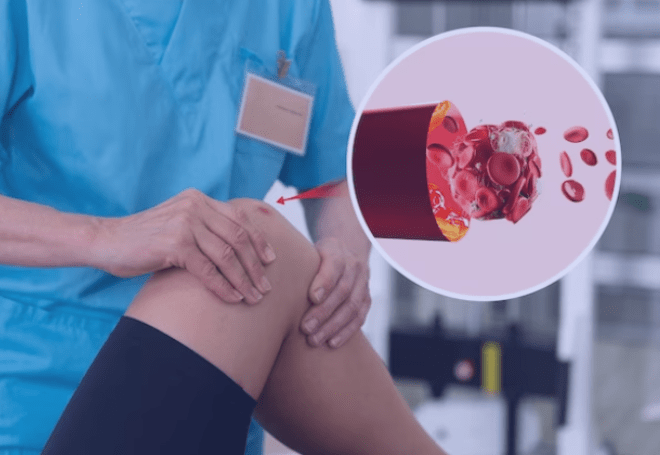
- The harvested donor cells are then infused into the recipient’s bloodstream. The transplanted stem cells travel to the recipient’s bone marrow, where they begin the process of producing new, healthy blood and immune cells.
Engraftment and Monitoring:
- Engraftment is the critical phase during which the transplanted cells establish themselves in the recipient’s bone marrow.
- Throughout this period, patients are closely monitored for signs of engraftment, as well as for potential complications such as GVHD, infections, and other side effects.
Potential for Graft-versus-Tumor Effect:
- Allo-BMT has the potential for a graft-versus-tumor effect, where the donor’s immune cells recognize and attack remaining cancer cells in the recipient.
Treatment for Genetic Disorders:
- Allo-BMT can be curative for certain genetic disorders by providing the recipient with healthy cells carrying the correct genetic information.
Larger Donor Pool:
- Allo-BMT allows for a broader donor pool, including siblings, unrelated donors, and, in some cases, umbilical cord blood.
Long-term Remission:
- In some cases, allogeneic transplantation offers the potential for long-term remission and, in the best scenarios, a cure for the underlying disease.
Allogeneic Bone Marrow Transplant represents a beacon of hope for individuals facing serious blood-related disorders and certain genetic conditions. The collaboration between donors and recipients, the advancements in transplant technology, and the vigilant care provided by healthcare teams contribute to the potential for successful outcomes. As research continues and our understanding of immunology deepens, allogeneic transplantation remains at the forefront of personalized medicine, offering the prospect of renewed health and a second chance at life.
Umbilical Cord Blood Transplant
Umbilical Cord Blood Transplant (UCBT) has emerged as a groundbreaking therapeutic option, utilizing the rich source of hematopoietic stem cells found in umbilical cord blood to treat various life-threatening diseases, particularly those affecting the blood and immune system. This innovative approach has redefined the landscape of transplantation, offering a readily available and less stringent alternative to traditional bone marrow or peripheral blood stem cell transplants.
Cell Count Limitations:
- Cord blood units contain a smaller number of stem cells compared to adult donor sources, which can affect the speed of engraftment.
Delayed Immune Reconstitution:
- The immaturity of cord blood cells may result in a longer time for the immune system to fully recover after transplantation.
Cord Blood Collection:
- Umbilical cord blood is collected immediately after the birth of a baby, posing no risk or discomfort to the newborn or the mother.
- The blood is drawn from the umbilical cord and placenta, which is typically discarded after childbirth.
Cord Blood Banking:
- The collected cord blood is processed and cryopreserved in cord blood banks, where it can be stored for long periods without losing its regenerative properties.
- This process creates a valuable inventory of cord blood units that can be accessed when needed for transplantation.
Donor Selection:
- Umbilical cord blood units can be used for allogeneic transplantation, meaning the donor is genetically different from the recipient.
- Due to the immature nature of cord blood cells, there is less strict matching criteria compared to other types of transplants, broadening the donor pool.
Preparative Regimen:
- Before the transplantation, the recipient undergoes a preparative regimen, which includes chemotherapy and sometimes radiation, to create space in the bone marrow for the cord blood cells to engraft.
Cord Blood Transplantation:
- The cryopreserved cord blood unit is thawed and infused into the recipient’s bloodstream, similar to a blood transfusion.
- The infused stem cells travel to the bone marrow and begin the process of producing new blood and immune cells.
Abundant Availability:
- Cord blood units are readily available in public cord blood banks, providing a diverse and extensive donor pool for patients in need.
Reduced Risk of Graft-versus-Host Disease (GVHD):
- Cord blood cells are immunologically immature, which may reduce the risk and severity of GVHD compared to adult donor transplants.
Low Risk of Transmissible Infections:
- Since cord blood is collected at birth, it is less likely to carry transmissible infections compared to adult donor sources.
Versatile Donor Pool:
- Cord blood transplants are suitable for patients who may not find a suitable match among adult donors, especially for individuals from diverse ethnic backgrounds.
Umbilical Cord Blood Transplant has carved a unique niche in the field of transplantation, offering a readily available and versatile source of hematopoietic stem cells. As medical research and technology advance, the potential applications and success rates of UCBT continue to improve, bringing hope to patients facing various hematological and genetic disorders. The small cord that once connected a newborn to life now holds the promise of renewed life for those in need, showcasing the remarkable potential of medical science and the impact of forward-thinking approaches to healthcare.
Haploidentical Donor Transplant
Haploidentical Donor Transplantation, or haplo transplant, has emerged as a revolutionary approach to stem cell transplantation, broadening the donor pool to include family members who are partially matched genetically. This innovative technique has overcome historical challenges associated with finding a fully matched donor, offering renewed hope to patients facing life-threatening hematological disorders. Let’s delve into the intricacies of haploidentical donor transplants and their transformative impact on the field of medicine.
Graft-versus-Host Disease (GVHD):
- Despite efforts to minimize GVHD, it remains a potential complication in haploidentical transplants. Advances in T-cell manipulation techniques aim to strike a balance between GVHD and GVT effects.
Infection Risk:
- Patients undergoing haploidentical transplantation may face a higher risk of infections during the early stages of immune system recovery.
Partial Genetic Match:
- In a haploidentical transplant, the donor is a family member (typically a parent, child, or sibling) who shares only half of the patient’s human leukocyte antigen (HLA) markers. This partial genetic match allows for a broader range of potential donors.
T-cell Depletion or Manipulation:
- To minimize the risk of graft-versus-host disease (GVHD), a condition where donor immune cells attack the recipient’s tissues, various techniques are employed.
- T-cell depletion or selective manipulation may be utilized to reduce the number of T cells in the donor graft, balancing the risk of GVHD with the need for effective graft-versus-tumor (GVT) activity.
Preparative Regimen:
- Before transplantation, the patient undergoes a preparative regimen, which typically involves chemotherapy and, in some cases, radiation therapy.
- The goal is to eliminate the patient’s diseased or malfunctioning cells, creating space for the donor cells to engraft and regenerate a healthy blood and immune system.
Stem Cell Transplantation:
- The harvested stem cells from the haploidentical donor are infused into the patient’s bloodstream, much like other stem cell transplant procedures.
- These stem cells migrate to the bone marrow, where they differentiate and begin producing new blood and immune cells.
Broader Donor Pool:
- Haploidentical transplants significantly expand the donor pool, as nearly every individual has a family member who is a potential haploidentical donor.
Timely Access to Transplantation:
- Finding a fully matched donor can be a time-consuming process. Haploidentical donors offer a more readily available option, allowing for faster transplantation and potentially improved outcomes.
Graft-versus-Tumor Effect:
- The partial genetic mismatch between donor and recipient may enhance the GVT effect, where the donor immune cells recognize and attack residual cancer cells in the recipient.
Reduced Relapse Risk:
- The enhanced immune response from haploidentical transplantation may contribute to a lower risk of disease relapse.
Haploidentical Donor Transplantation has transformed the landscape of stem cell transplantation, offering a viable and accessible option for patients in need. The delicate balance between donor and recipient genetics, coupled with advances in immune modulation, has opened new avenues for treating hematological disorders. As research and clinical experience continue to refine haploidentical transplant protocols, this approach stands as a testament to the resilience of innovation in medical science, providing renewed hope and improved outcomes for patients facing challenging diagnoses.
Reduced Intensity Transplant
Reduced Intensity Transplant (RIT), also known as non-myeloablative or mini-transplant, represents a groundbreaking evolution in stem cell transplantation. This innovative approach is designed to make the transplant process more accessible for patients who may not tolerate the intense conditioning regimens associated with traditional transplants. Let’s explore the intricacies of Reduced Intensity Transplant and its transformative impact on the treatment of various hematologic disorders.
Risk of Disease Relapse:
- The reduced intensity of the preparative regimen may be associated with a higher risk of disease relapse compared to standard transplants.
Balancing GVT and GVHD:
- Achieving a delicate balance between the graft-versus-tumor effect and minimizing the risk of graft-versus-host disease (GVHD) remains a critical consideration.
Gentler Preparative Regimen:
- In contrast to the high-dose chemotherapy and radiation used in traditional transplants, Reduced Intensity Transplantation employs a less aggressive preparative regimen.
- The goal is not to completely obliterate the patient’s bone marrow but rather to create enough space for the donor cells to engraft and coexist with the patient’s remaining cells.
Targeted Immune System Suppression:
- Reduced Intensity Transplants rely on targeted immune system suppression rather than complete ablation.
- This allows for a milder preparative regimen, reducing the risk of severe side effects and making the transplant approachable for older patients or those with underlying health conditions.
Stem Cell Transplantation:
- The donor’s stem cells are infused into the patient’s bloodstream, similar to other types of stem cell transplants.
- These stem cells find their way to the bone marrow, where they gradually establish and begin producing new blood and immune cells.
Graft-versus-Tumor Effect:
- The reduced intensity of the preparative regimen may still allow for a graft-versus-tumor (GVT) effect, where the donor immune cells recognize and attack cancer cells in the recipient.
Suitability for Older Patients:
- Reduced Intensity Transplants are often considered for older patients who may not tolerate the intense conditioning regimens associated with traditional transplants.
Expanded Eligibility for Patients with Comorbidities:
- Patients with certain pre-existing health conditions, who may be at higher risk for complications with standard transplants, may find Reduced Intensity Transplantation to be a more feasible option.
Shortened Recovery Time:
- The milder preparative regimen typically results in a shorter recovery time, allowing patients to return to their normal activities sooner.
Lower Risk of Transplant-related Mortality:
- Reduced Intensity Transplants are associated with a lower risk of transplant-related mortality, making the procedure more favorable for certain patient populations.
Reduced Intensity Transplantation represents a significant advancement in stem cell transplantation, offering a gentler alternative for patients who may face challenges with more aggressive approaches. As the field continues to evolve, research and clinical experience will refine the protocols for Reduced Intensity Transplants, making this method increasingly accessible and effective for a broader range of patients. This nuanced approach to transplantation exemplifies the commitment of medical science to improving outcomes and quality of life for individuals facing hematologic disorders.
Lymphoma BMT Cancer Program
The Lymphoma Blood and Marrow Transplant (BMT) Cancer Program represents a beacon of hope and progress in the field of oncology. Specifically tailored for individuals facing lymphoma, a group of blood cancers that affect the lymphatic system, this comprehensive program integrates the power of bone marrow transplantation with cutting-edge advancements in cancer treatment. Let’s explore the key components and benefits of the Lymphoma BMT Cancer Program.
Lymphoma is a diverse group of cancers that originate in the lymphatic system, affecting lymphocytes—the infection-fighting cells of the immune system. The two main types of lymphoma are Hodgkin lymphoma and non-Hodgkin lymphoma, each with various subtypes. While many individuals respond well to standard treatments, those with high-risk or relapsed lymphomas may find hope in the innovative approaches offered by the Lymphoma BMT Cancer Program.
Patient Evaluation and Eligibility:
- The program begins with a thorough evaluation of the patient’s medical history, overall health, and specific characteristics of the lymphoma.
- Eligibility for the Lymphoma BMT Cancer Program is determined based on factors such as disease stage, response to previous treatments, and the overall health of the patient.
Specialized Treatment Planning:
- Oncologists and hematologists collaborate to create an individualized treatment plan, incorporating bone marrow transplantation as a key component.
- The treatment plan may involve high-dose chemotherapy, radiation therapy, and stem cell transplantation, aiming to eradicate cancer cells and reset the immune system.
Bone Marrow or Stem Cell Harvesting:
- For autologous transplants, the patient’s own stem cells may be harvested and stored before the intensified treatment begins.
- In allogeneic transplants, stem cells from a compatible donor—potentially a family member or unrelated donor—are collected for transplantation.
Preparative Regimen:
- Patients undergo a preparative regimen involving high-dose chemotherapy and, in some cases, radiation therapy.
- This intensive treatment aims to eliminate cancerous cells and create a favorable environment for the transplanted cells to engraft.
Bone Marrow Transplantation:
- Autologous or allogeneic bone marrow transplantation is performed, involving the infusion of harvested stem cells into the patient’s bloodstream.
- The transplanted cells migrate to the bone marrow and initiate the production of healthy blood and immune cells.
Increased Cure Rates:
- The Lymphoma BMT Cancer Program has shown promising results, especially in patients with high-risk or relapsed lymphomas, potentially leading to increased cure rates.
Minimized Risk of Disease Relapse:
- The intensity of the preparative regimen, combined with the graft-versus-tumor effect in allogeneic transplants, aims to minimize the risk of disease relapse.
Individualized Care:
- The program emphasizes personalized treatment plans, considering the unique characteristics of each patient’s lymphoma and tailoring the approach accordingly.
Access to Clinical Trials:
- Patients within the Lymphoma BMT Cancer Program may have the opportunity to participate in clinical trials, contributing to ongoing advancements in lymphoma research and treatment.
The Lymphoma BMT Cancer Program stands at the forefront of progress in cancer care, providing individuals with lymphoma new avenues for treatment and hope for a healthier future. As research continues and the program evolves, it exemplifies the commitment of medical professionals to pushing the boundaries of what is possible in the fight against lymphoma. This comprehensive and integrative approach represents a powerful collaboration between science, medicine, and the unwavering resilience of those facing lymphoma.
Hematopoietic Stem Cell Transplantation
Hematopoietic Stem Cell Transplantation (HSCT), often referred to as bone marrow transplantation, stands as a transformative medical procedure that holds the potential to cure or manage a range of life-threatening blood disorders and certain cancers. This innovative approach involves the infusion of healthy hematopoietic stem cells (HSCs) into a patient, enabling the regeneration of a functional blood and immune system. Let’s delve into the intricacies of Hematopoietic Stem Cell Transplantation and its profound impact on the landscape of medical care.
Hematopoietic stem cells (HSCs) are unique cells found in the bone marrow and peripheral blood. They have the remarkable ability to differentiate into various types of blood cells, including red blood cells, white blood cells, and platelets. These cells play a crucial role in maintaining the body’s blood and immune system.
Indications for Hematopoietic Stem Cell Transplantation: HSCT is a viable treatment option for a range of diseases, including:
Leukemia: HSCT is often used to treat acute and chronic forms of leukemia, where abnormal blood cells crowd out healthy cells.
Lymphoma: Both Hodgkin’s and non-Hodgkin’s lymphomas can be treated with HSCT, especially in cases of relapse or when standard treatments are ineffective.
Multiple Myeloma: This form of cancer affects plasma cells in the bone marrow, and HSCT can be a valuable therapeutic option.
Aplastic Anemia: In cases where the bone marrow fails to produce enough blood cells, HSCT can help restore normal blood cell production.
Sickle Cell Anemia: HSCT can provide a potential cure for sickle cell disease by replacing defective stem cells with healthy ones.
The transplantation process involves several key steps:
Harvesting Stem Cells: HSCs can be sourced from the patient (autologous transplant), a compatible family member (allogeneic transplant), or a compatible unrelated donor.
Conditioning Therapy: Before the transplant, patients undergo conditioning therapy, which involves high-dose chemotherapy or radiation to eliminate diseased cells and create space for the new stem cells.
Transplantation: The harvested stem cells are infused into the patient’s bloodstream, and they travel to the bone marrow, where they begin to multiply and generate healthy blood cells.
Recovery: Post-transplant, patients require close monitoring and care to manage potential complications such as infections and graft-versus-host disease (GVHD) in allogeneic transplants.
HSCT has offered a new lease on life for countless individuals, leading to remarkable success stories of patients who have overcome life-threatening diseases. However, challenges such as finding suitable donors, managing transplant-related complications, and the risk of graft rejection remain significant hurdles in making HSCT universally accessible.
Hematopoietic Stem Cell Transplantation stands at the forefront of medical advancements, providing hope and healing for those facing life-threatening hematologic disorders. As research continues and technology evolves, the potential for further success in treating a broader range of diseases through HSCT becomes increasingly promising, marking a transformative era in the field of medicine.
