Chronic Myeloid Leukemia
Chronic Myeloid Leukemia (CML) is a type of cancer that affects the blood and bone marrow. It is a form of leukemia characterized by the uncontrolled growth of myeloid cells, which are responsible for producing red blood cells, platelets, and white blood cells. This content aims to provide a comprehensive overview of CML, including its causes, symptoms, diagnosis, and treatment options.
CML is often associated with a genetic abnormality known as the Philadelphia chromosome. This chromosome results from a translocation between chromosomes 9 and 22, leading to the formation of a fusion gene called BCR-ABL. The presence of this gene is a hallmark of CML and plays a crucial role in the development of the disease.
Symptoms:
The symptoms of CML can vary from person to person, and some individuals may not exhibit any symptoms during the early stages. Common symptoms include fatigue, weakness, weight loss, night sweats, and an enlarged spleen or liver. As the disease progresses, CML may lead to an increased risk of infections, easy bruising or bleeding, and bone pain.
CML is generally classified into three phases: chronic phase, accelerated phase, and blast phase. Most individuals are diagnosed in the chronic phase, which is characterized by the slow progression of the disease. If left untreated, CML may progress to the accelerated phase and eventually to the blast phase, which is more aggressive and resembles acute leukemia.
With advancements in treatment, the prognosis for individuals with CML has significantly improved. Many patients can achieve long-term remission and lead normal, productive lives with proper medical management. Regular monitoring and follow-up with healthcare professionals are essential to ensure the effectiveness of the chosen treatment plan.
Chronic Myeloid Leukemia is a complex and challenging disease, but advancements in medical research and treatment options have provided hope for those affected. Early diagnosis, combined with targeted therapies, has transformed CML into a manageable condition for many individuals. Ongoing research continues to enhance our understanding of the disease and improve treatment outcomes, offering optimism for the future.
Anemia
Anemia is a common medical condition characterized by a deficiency of red blood cells or hemoglobin in the blood, leading to a reduced ability to carry oxygen to body tissues. This content aims to provide a comprehensive overview of anemia, exploring its causes, symptoms, types, and available management options.
Anemia can result from various factors, including nutritional deficiencies (such as iron, vitamin B12, or folic acid), chronic diseases (like chronic kidney disease or inflammatory disorders), genetic conditions (like thalassemia or sickle cell anemia), and bone marrow disorders. Additionally, certain medications, infections, and autoimmune disorders can contribute to the development of anemia.
Symptoms:
The symptoms of anemia can vary in severity and may include fatigue, weakness, pale skin, shortness of breath, dizziness, headache, cold hands and feet, and an irregular heartbeat. Individuals with anemia may also experience difficulty concentrating and a decreased ability to perform physical activities due to the reduced oxygen-carrying capacity of their blood.
There are several types of anemia, each with its own specific causes and characteristics. Common types include:
Iron-deficiency anemia: Caused by insufficient iron intake or absorption, often due to poor diet, blood loss (through menstruation or gastrointestinal bleeding), or pregnancy.
Vitamin-deficiency anemia: Resulting from deficiencies in vitamins such as B12, B6, and folic acid, which are essential for red blood cell production.
Hemolytic anemia: Occurs when red blood cells are destroyed faster than the body can replace them, leading to a shortage of healthy red blood cells.
Aplastic anemia: Stem cells in the bone marrow are damaged, leading to a reduced production of red blood cells.
Sickle cell anemia: A genetic disorder causing red blood cells to become misshapen and break down more easily, leading to a chronic shortage of healthy red blood cells.
The treatment of anemia depends on its underlying cause. Common management strategies include:
Iron supplementation: For iron-deficiency anemia, iron supplements may be prescribed to replenish iron levels.
Vitamin supplements: Deficiencies in vitamin B12, B6, or folic acid may be addressed through supplementation.
Blood transfusions: In severe cases or emergencies, blood transfusions may be necessary to quickly boost red blood cell levels.
Erythropoiesis-stimulating agents: Medications that stimulate the production of red blood cells in the bone marrow may be prescribed in certain cases.
Treating underlying conditions: Addressing the root cause of anemia, such as managing chronic diseases or stopping the use of medications contributing to anemia.
Anemia is a widespread condition that can impact individuals of all ages and backgrounds. Early detection, proper diagnosis, and appropriate management are crucial for improving symptoms and preventing complications. Individuals experiencing symptoms of anemia should seek medical attention for a thorough evaluation and personalized treatment plan. With the right interventions, many cases of anemia can be effectively managed, allowing individuals to lead healthy and active lives.
Acute Lymphoblastic Leukemia
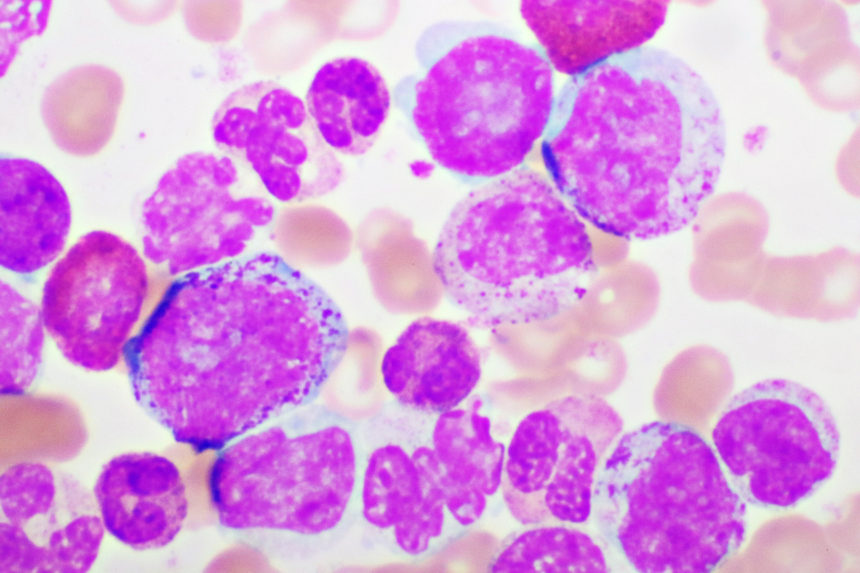
Acute Lymphoblastic Leukemia (ALL) is a rapidly progressing cancer that affects the blood and bone marrow, primarily characterized by the uncontrolled proliferation of immature lymphocytes. This content aims to provide an in-depth understanding of ALL, including its causes, symptoms, diagnostic methods, and available treatment options.
The exact cause of ALL is not fully understood, but certain risk factors may contribute to its development. These risk factors include genetic predisposition, exposure to high doses of radiation, certain genetic syndromes (such as Down syndrome), and exposure to certain chemicals and medications. However, in many cases, ALL arises sporadically without an identifiable cause.
Symptoms:
ALL symptoms can manifest rapidly, and they may vary among individuals. Common symptoms include fatigue, weakness, pale skin, frequent infections, unexplained bruising or bleeding, joint pain, and swollen lymph nodes. Children with ALL may also experience a decreased appetite, weight loss, and irritability.
Diagnosing ALL involves a combination of medical history review, physical examination, and laboratory tests. Blood tests, including a complete blood count (CBC) and peripheral blood smear, can reveal abnormal levels of white blood cells, red blood cells, and platelets. Bone marrow aspiration and biopsy are often performed to confirm the diagnosis and determine the extent of the disease.
Subtypes of ALL: There are different subtypes of ALL based on the specific type of lymphocytes affected and the genetic characteristics of the leukemia cells. Subtyping is crucial for developing targeted treatment plans and predicting prognosis.
Treatment:
The treatment approach for ALL typically involves multiple phases and may include:
Induction Therapy: Intensive chemotherapy is administered to achieve remission by eliminating as many leukemia cells as possible.
Consolidation Therapy: Additional chemotherapy is given to eliminate any remaining leukemia cells and prevent a relapse.
Maintenance Therapy: Lower doses of chemotherapy are provided over an extended period to prevent the recurrence of leukemia.
Stem Cell Transplant: In some cases, a stem cell transplant may be recommended, especially for individuals with high-risk or relapsed ALL. This involves replacing diseased bone marrow with healthy stem cells.
Targeted Therapies: Emerging targeted therapies, such as tyrosine kinase inhibitors, may be used in specific cases, particularly when certain genetic mutations are present.
Advances in treatment have significantly improved the prognosis for individuals with ALL, especially in children. The outlook depends on factors such as age, overall health, response to treatment, and specific genetic characteristics of the leukemia cells. Ongoing medical monitoring is crucial for managing potential side effects and monitoring for any signs of relapse.
Acute Lymphoblastic Leukemia is a challenging and aggressive form of cancer, but advancements in medical research and treatment options offer hope for many individuals. Early diagnosis and prompt initiation of appropriate therapies play a pivotal role in improving outcomes. Collaborative efforts between healthcare professionals and patients are essential to navigating the complexities of ALL and achieving the best possible results in the fight against this form of leukemia.
Chronic Lymphocytic Leukemia
Chronic Lymphocytic Leukemia (CLL) is a type of cancer that affects the blood and bone marrow, characterized by the gradual accumulation of abnormal lymphocytes, a type of white blood cell. This content aims to provide a thorough understanding of CLL, covering its causes, symptoms, diagnosis, and available treatment options.
The exact cause of CLL is not fully understood, but certain risk factors may contribute to its development. These factors include age, family history of CLL, exposure to certain chemicals and environmental factors, and a history of certain infections such as the Epstein-Barr virus. CLL is more common in older adults, and men are slightly more likely to develop the disease than women.
Symptoms:
CLL often progresses slowly, and individuals may not experience symptoms in the early stages. Common symptoms, when present, may include fatigue, weakness, enlarged lymph nodes, unexplained weight loss, night sweats, and frequent infections. Due to its slow progression, some individuals may be diagnosed incidentally during routine blood tests.
The diagnosis of CLL involves a combination of medical history review, physical examination, and laboratory tests. Blood tests, including a complete blood count (CBC) and flow cytometry, help identify an elevated number of abnormal lymphocytes. A bone marrow biopsy may be performed to confirm the diagnosis and assess the extent of bone marrow involvement.
CLL is typically staged using systems like the Rai or Binet staging systems, which classify the disease into different stages based on the number of affected lymph nodes, liver, and spleen, as well as the presence of anemia or thrombocytopenia.
Treatment:
The decision to initiate treatment for CLL depends on various factors, including the stage of the disease, symptoms, and overall health. Treatment options may include:
Watch and Wait: In many cases, especially in the early stages, CLL may not require immediate treatment. Regular monitoring is conducted, and treatment is initiated if the disease progresses.
Chemotherapy: Traditional chemotherapy drugs may be used, particularly in more advanced stages of CLL.
Immunotherapy: Monoclonal antibodies, such as rituximab or obinutuzumab, can be used to target specific proteins on the surface of CLL cells.
Targeted Therapies: Drugs like ibrutinib, venetoclax, and idelalisib are targeted therapies that interfere with specific pathways involved in the growth of CLL cells.
Stem Cell Transplant: In certain cases, particularly for younger and healthier individuals, a stem cell transplant may be considered.
CLL is generally a slowly progressing disease, and many individuals live for years without requiring treatment. The prognosis varies, and factors such as the stage of CLL, genetic characteristics, and overall health influence outcomes. Advances in treatment have significantly improved survival rates, and ongoing research continues to enhance therapeutic options.
Conclusion:
Chronic Lymphocytic Leukemia is a complex disease that requires individualized management based on various factors. Regular communication between healthcare professionals and patients is essential to determine the most appropriate course of action. With advancements in treatment and ongoing research, individuals diagnosed with CLL can lead fulfilling lives with appropriate medical care and support.
Hairy Cell Leukemia
Hairy Cell Leukemia (HCL) is a rare, chronic form of leukemia characterized by the abnormal growth of B cells in the bone marrow and spleen. Despite its rarity, HCL has a distinct set of features that differentiate it from other types of leukemia. This content aims to provide an overview of Hairy Cell Leukemia, including its causes, symptoms, diagnosis, and available treatment options.
Diagnosing Hairy Cell Leukemia involves a series of tests, including:
- Blood Tests: A complete blood count (CBC) may reveal abnormalities in the number and appearance of blood cells.
- Bone Marrow Biopsy: This involves the removal of a small sample of bone marrow for examination under a microscope.
- Imaging Studies: CT scans or ultrasounds may be used to assess the size of the spleen and liver.
Causes:
The exact cause of Hairy Cell Leukemia remains unknown. However, certain risk factors may contribute to its development. These risk factors include exposure to certain chemicals or toxins, such as benzene, and a history of certain infections like the human T-cell leukemia virus (HTLV-1).
Symptoms:
Hairy Cell Leukemia often progresses slowly, and its symptoms may develop gradually. Common symptoms include:
- Fatigue: Patients with HCL often experience persistent fatigue and weakness.
- Enlarged Spleen and Liver: The abnormal accumulation of hairy cells can lead to the enlargement of the spleen and liver.
- Easy Bruising and Bleeding: HCL can affect the production of healthy blood cells, leading to easy bruising and an increased risk of bleeding.
- Frequent Infections: The compromised immune system in HCL patients may result in an increased susceptibility to infections.
- Pain or Discomfort: Some individuals with Hairy Cell Leukemia may experience pain or discomfort in the abdomen due to the enlargement of organs.
Hairy Cell Leukemia is a chronic condition, and treatment is typically initiated when symptoms become bothersome or if complications arise. Common treatment options include:
- Chemotherapy: The use of specific drugs to kill or slow the growth of leukemia cells.
- Immunotherapy: Monoclonal antibodies, such as rituximab, target specific proteins on the surface of hairy cells.
- Interferon Therapy: Interferon-alpha may be used to stimulate the immune system and slow the growth of leukemia cells.
- Targeted Therapies: Newer drugs, such as cladribine and pentostatin, specifically target the abnormal cells in HCL.
Hairy Cell Leukemia, though rare, requires careful management and treatment. Advances in medical research continue to improve our understanding of the disease, leading to more targeted and effective treatment options. Individuals diagnosed with HCL can benefit from a comprehensive approach that combines medical treatment, symptom management, and ongoing monitoring to ensure the best possible outcome and quality of life. If you or someone you know is experiencing symptoms suggestive of Hairy Cell Leukemia, it is crucial to consult with a healthcare professional for a proper diagnosis and personalized treatment plan.
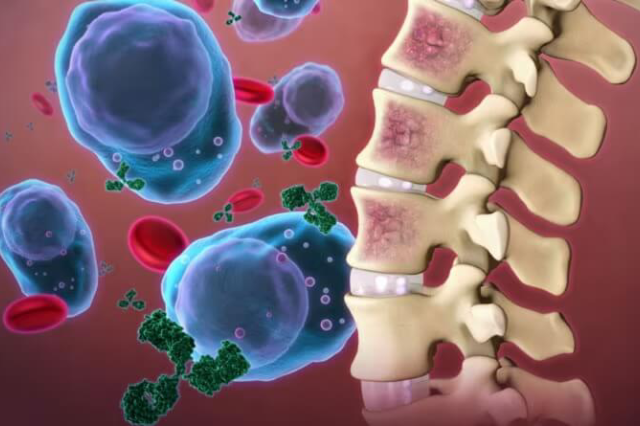
Multiple Myeloma
Multiple Myeloma is a complex and relatively uncommon form of cancer that affects plasma cells, a type of white blood cell responsible for producing antibodies. This content aims to shed light on the essential aspects of Multiple Myeloma, including its characteristics, common symptoms, diagnostic processes, and available treatment options.
Multiple Myeloma is characterized by the abnormal proliferation of plasma cells in the bone marrow. These cancerous cells can crowd out normal blood cells, leading to a range of complications. The disease can affect multiple areas of the body, including bones, bone marrow, and sometimes other organs.
Symptoms:
The symptoms of Multiple Myeloma can vary, and some individuals may not experience noticeable symptoms in the early stages. Common symptoms include:
- Bone Pain: Persistent pain, especially in the back, hips, and skull, is a common early symptom due to the weakening of bones.
- Fatigue: Anemia caused by a reduction in red blood cells can lead to fatigue and weakness.
- Kidney Problems: Multiple Myeloma can affect the kidneys, causing symptoms such as increased thirst, frequent urination, and fluid retention.
- Frequent Infections: Weakened immune function may result in an increased susceptibility to infections.
- Unexplained Weight Loss: Rapid and unintentional weight loss may occur in some cases.
Diagnosis:
Diagnosing Multiple Myeloma involves a series of tests, including:
- Blood Tests: A complete blood count (CBC) can reveal abnormalities in the number and type of blood cells.
- Bone Marrow Biopsy: A small sample of bone marrow is extracted and examined under a microscope to detect abnormal plasma cells.
- Imaging Studies: X-rays, CT scans, or MRIs can identify bone lesions and assess the extent of the disease.
The management of Multiple Myeloma typically involves a combination of therapies tailored to the individual patient. Common treatment options include:
- Chemotherapy: Powerful drugs are used to target and destroy cancer cells.
- Immunomodulatory Drugs: Drugs like thalidomide, lenalidomide, and pomalidomide enhance the immune system’s ability to combat cancer.
- Proteasome Inhibitors: Medications such as bortezomib and carfilzomib interfere with the normal breakdown of proteins in cancer cells.
- Stem Cell Transplantation: High-dose chemotherapy is followed by the infusion of the patient’s own stem cells to rebuild healthy bone marrow.
- Targeted Therapies: Monoclonal antibodies like daratumumab and elotuzumab target specific proteins on myeloma cells.
Multiple Myeloma poses unique challenges due to its impact on the bone marrow and various organs. Advances in research and treatment options have significantly improved outcomes for individuals with this condition. A multidisciplinary approach involving oncologists, hematologists, and other healthcare professionals is crucial for developing personalized treatment plans that address the specific needs of each patient. If you or someone you know is experiencing symptoms indicative of Multiple Myeloma, seeking prompt medical attention and consultation with healthcare professionals is vital for an accurate diagnosis and timely initiation of appropriate treatment.
Blood Cancer
Blood cancer, also known as hematologic cancer, encompasses a diverse group of cancers that affect the blood, bone marrow, and lymphatic system. This content aims to provide a comprehensive overview of blood cancer, covering its various types, potential causes, common symptoms, and available treatment options.
Leukemia:
- Acute Lymphoblastic Leukemia (ALL)
- Acute Myeloid Leukemia (AML)
- Chronic Lymphocytic Leukemia (CLL)
- Chronic Myeloid Leukemia (CML)
Lymphoma:
- Hodgkin Lymphoma
- Non-Hodgkin Lymphoma
Myeloma:
- Multiple Myeloma
Causes:
The exact causes of blood cancer are often unknown, but several factors may contribute to its development:
- Genetic predisposition
- Exposure to certain chemicals or toxins
- Radiation exposure
- Viral infections, such as the Epstein-Barr virus (linked to some lymphomas)
- Immune system disorders
Symptoms:
Symptoms of blood cancer can vary depending on the type and stage of the disease. Common symptoms include:
- Persistent fatigue and weakness
- Unexplained weight loss
- Frequent infections
- Easy bruising or bleeding
- Enlarged lymph nodes or spleen
- Bone pain or tenderness
Diagnosis:
Diagnosing blood cancer involves a combination of medical history assessment, physical examination, and various tests:
- Blood tests, including complete blood count (CBC)
- Bone marrow biopsy
- Imaging studies (X-rays, CT scans, PET scans)
- Lymph node biopsy for lymphomas
Treatment:
Treatment approaches for blood cancer depend on the type, stage, and individual patient factors:
- Chemotherapy: Uses drugs to kill or control cancer cells.
- Immunotherapy: Enhances the body’s immune system to target and destroy cancer cells.
- Targeted Therapy: Targets specific molecules involved in cancer cell growth.
- Stem Cell Transplantation: Replaces diseased or damaged bone marrow with healthy stem cells.
- Radiation Therapy: Uses high-energy rays to target and kill cancer cells.
Blood cancer is a complex and diverse group of diseases that require tailored treatment approaches. Advances in medical research and technology have significantly improved outcomes, offering hope to individuals diagnosed with these conditions. Early detection, accurate diagnosis, and a multidisciplinary treatment plan involving oncologists, hematologists, and other specialists play a crucial role in managing and overcoming blood cancer. If you or someone you know is experiencing symptoms suggestive of blood cancer, seeking prompt medical attention and consulting with healthcare professionals is essential for timely diagnosis and effective treatment.
Leukemia & Lymphoma
Leukemia and lymphoma are two distinct yet interconnected types of blood cancers, each with its unique characteristics, affecting the blood, bone marrow, and lymphatic system. This content aims to unravel the complexities of leukemia and lymphoma, shedding light on their types, causes, symptoms, and available treatment options.
Diagnosis:
Diagnosis involves a series of tests, including blood tests, bone marrow biopsy, imaging studies, and lymph node biopsy, to determine the type and extent of the cancer.
Treatment:
Treatment strategies vary based on the type and stage of the disease and may include:
- Chemotherapy
- Immunotherapy
- Targeted therapy
- Stem cell transplantation
- Radiation therapy
Causes:
The precise causes of leukemia and lymphoma are not fully understood, but certain risk factors may contribute:
- Genetic predisposition
- Exposure to certain chemicals or toxins
- Radiation exposure
- Viral infections (e.g., Epstein-Barr virus for some lymphomas)
- Immune system disorders
Symptoms:
Common symptoms of leukemia and lymphoma include:
- Persistent fatigue and weakness
- Unexplained weight loss
- Frequent infections
- Easy bruising or bleeding
- Enlarged lymph nodes or spleen
- Bone pain or tenderness
Leukemia and lymphoma pose significant challenges, but advancements in research and treatment have greatly improved outcomes. A personalized and multidisciplinary approach involving healthcare professionals is essential for managing these blood cancers effectively. Early detection, accurate diagnosis, and timely intervention play pivotal roles in providing individuals with leukemia and lymphoma the best chance for successful treatment and improved quality of life. If you or someone you know experiences symptoms indicative of these blood cancers, seeking prompt medical attention is crucial for a thorough evaluation and appropriate management.
Polycythemia Vera
Polycythemia Vera (PV) is a rare but serious blood disorder characterized by the overproduction of red blood cells in the bone marrow. This condition falls under the umbrella of myeloproliferative neoplasms, a group of disorders where the bone marrow produces excessive blood cells. PV is a chronic condition that requires careful management to prevent complications.
Diagnosing PV requires a comprehensive approach, combining clinical findings, laboratory results, and sometimes imaging studies. The identification of the JAK2 mutation and characteristic bone marrow changes play crucial roles in confirming the diagnosis. A prompt and accurate diagnosis is essential for initiating appropriate treatment and management strategies for individuals with Polycythemia Vera. If PV is suspected, individuals should seek consultation with a hematologist or a healthcare professional with expertise in blood disorders for a thorough evaluation.
Causes:
The exact cause of Polycythemia Vera is not well understood, but it is often linked to a genetic mutation called JAK2 (Janus kinase 2) mutation. This mutation leads to the continuous signaling for the bone marrow to produce more blood cells, resulting in an increased number of red blood cells.
Symptoms:
Increased Blood Viscosity: The surplus of red blood cells can cause the blood to become thicker, leading to a higher risk of blood clots.
Fatigue and Weakness: Due to the increased viscosity of the blood, oxygen delivery to tissues may be compromised, resulting in fatigue and weakness.
Enlarged Spleen and Liver: The excess blood cells can cause the spleen and liver to enlarge, leading to abdominal discomfort.
Headaches and Dizziness: Impaired blood flow and oxygen delivery to the brain can cause headaches and dizziness.
Bleeding and Bruising: Despite an increase in red blood cells, the presence of dysfunctional platelets can lead to bleeding and bruising issues.
Polycythemia Vera requires lifelong management to control symptoms and prevent complications. With advancements in medical understanding and treatment options, individuals diagnosed with PV can lead fulfilling lives with proper medical supervision. Early diagnosis and proactive management are crucial for maintaining a good quality of life for those affected by this rare blood disorder. If you suspect you may have symptoms of PV, it is important to consult with a healthcare professional for a thorough evaluation and appropriate management.