Bone Marrow Transplant (BMT)
Bone Marrow Transplant (BMT) or the Hematopoietic Stem Cell Transplant (HSCT) is the treatment process in which the diseased marrow of recipient is replaced by normal stem cells from the healthy donor or from the patient himself or herslf.
The marrow of recipient is first destroyed by chemotherapy ± Total Body Irradiation (TBI) ± Immunotherapy and then the stem cells are infused just like blood transfusion through central line. There is no surgery involved in the whole BMT process. After infusion the stem cells find their way to bone marrow and gets engrafted (start to work).
Types of BMT
Autologous BMT – here the stem cell source is from the patient self.
Autologous BMT
Autologous BMT: In this stem cell source is the patient themselves. Two principles are utilized in this type of BMT.
High Dose Therapy followed by stem cell rescue: For diseases like myeloma and relapsed lymphoma, the principle of ASCT is high dose chemotherapy followed by stem cell rescue. In these cases the patients are given high dose chemotherapy to get long term control of the disease.
Resetting immune system: Another principle in ASCT is providing strong immune suppression by chemo/immunotherapy and thereby resetting the immune system. This resetting of immune system makes the formation of new lymphocytes which may not be auto-reactive (not destroying own cells). This principle is being utilized for treating Autoimmune diseases like Multiple Sclerosis, Systemic Sclerosis, Dermatomyositis, SLE and others.
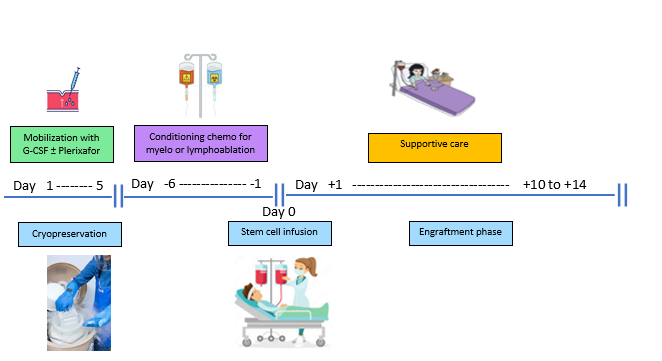
Mobilization and Collection of stem cells:
- In autologous BMT, the stem cells are collected from peripheral blood after mobilizing with G-CSF ± Plerixafor (given in the skin).
- Stem cells from peripheral blood may be collected by peripheral canula or HD catheter in central vein.
- Collection process is done by apheresis machine and it usually takes 4-6 hrs. the machine only collects stem cells and remaining cells are pushed back to into the body.
- Once adequate dose is achieved it is cryopreserved in liquid nitrogen at -180 °C.
- In case of myeloma, the conditioning is only for 1 day so cryopreservation is not needed.
Conditioning chemotherapy:
- High dose chemotherapy with or without immunotherapy is given to wipe out the recipient marrow and any residual tumor (myeloablative) or immune system (lymphoablative).
- In case of myeloma the conditioning regimen is single dose Inj Melphalan.
Reinfusion of stem cells:
- Once chemotherapy is over the stem cells are reinfused through the central vein (after thawing in case of cryopreserved stem cells).
Engraftment:
- Usually it takes 10-14 days for the stem cells to regenerate and restore the hematopoiesis and during this phase the patient is given supportive treatment in the form of blood product transfusion, antimicrobials and other treatments.
- Patients are also monitored for any change in the vital parameters.
Allogenic BMT
In this type of BMT the recipient’s bone marrow is replaced by donor’s normal marrow. Two types of principles are utilized in this type of BMT.
Graft versus Leukemia effect: In the allogenic BMT the recipient’s hematopoietic system is replaced by donor’s and in this process he gets the new immune system of donor’s. This new immune system will stay in the recipient and fight against the new developing cancer cells and this is called the GVL effect (Graft versus Leukemia/Tumor) throughout the life of patient.
Replacement of defective system: This principle is being utilized for treating defective marrow which can be acquired or genetic. Acquired disease are aplastic anemia, Paroxysmal Nocturnal Hemoglobinuria (PNH), etc. Genetic diseases are defective red cell disorders (Thalassemia, Sickle Cell Disease, etc.), Platelet disorders, Primary Immunodeficiency diseases or inborn errors of metabolism (enzyme defects, etc.).
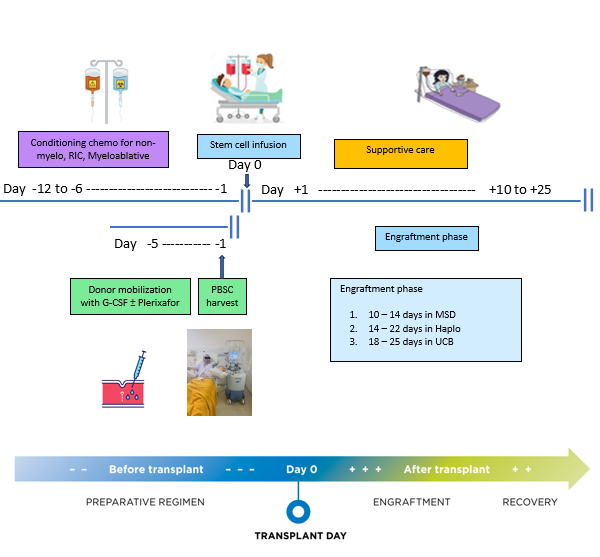
Conditioning chemotherapy ± TBI or immunotherapy:
- The intensity of conditioning therapy can be non-myeloablative to reduced intensity to myeloablative. This is decided by the transplant doctor and depends on many factor like disease, patient’s performance score, etc.
Mobilization and Collection of stem cells:
- In allogenic BMT, the stem cells are collected from the donor through peripheral blood after mobilizing with G-CSF ± Plerixafor (given in the skin).
- Stem cells from peripheral blood may be collected by peripheral canula or HD catheter in central vein.
- Collection process is done by apheresis machine and it usually takes 4-6 hrs. the machine only collects stem cells and remaining cells are pushed back to into the body.
- Usually the collection process from donor happens on day -1 (1 day before the infusion)
Reinfusion of stem cells:
- Once chemotherapy is over the stem cells are reinfused through the central vein.This day is called Day 0.
Engraftment:
- During this phase the stem cells regenerate and restore the hematopoiesis and the patient is given supportive treatment in the form of blood product transfusion, antimicrobials and other treatments.
- Days to engraft depends on the source of stem cells like 10-14 days for matched sibling/family donor, 14-20 days in case of Haplo donor and 20-25 days in case of cord blood donor.
What are the possible complications of BMT ?
- During conditioning phase : Side effects related to chemotherapy and these are dependent on the intensity and type of medicine. The usual side effects are nausea, vomiting, allergic reactions, fluid overload.
-
During engraftment phase
• Fever and infections (bacterial, viral or fungal).
• Bleeding and weakness
• Mucositis, which can lead to throat pain, abdominal pain, nausea and diarrhea.
• Regimen related toxicity can affect any organ
- During stem cell infusion : Stem cell infusion can cause allergic reactions, fluid overload and can cause cardiac side effects like arrhythmias with cryopreserved product transfusion.
-
During later phase after engraftment :
• The patient can develop acute GVHD (Graft Versus Host Disease), in which the donor Lymphocytes show reaction against the host tissue and it need prompt treatment initiation.
• Infections esp viral
• Chronic GVHD can affect any organ
Timing of BMT
- Usually for malignant diseases (blood cancers), BMT is done when the disease is in remission as the outcome of BMT is best in this state. However in resistant cases the BMT can still be done with partial remission state also, but these things need to be discussed in detail with the transplant physician. For non-malignant cases, it is preferable to do early BMT before any permanent organ damage is done. In genetic diseases like thalassemia and sickle cell disease, the best outcomes are for age 1 yr and 10 yrs. For primary immune deficiency disease it is done even at lesser than 1 yr age.
Preparation for BMT
- Once it is decided to go for BMT treatment, First and foremost thing needed is the HLA typing of the patient and all the potential donors which are initially the siblings and then extended family typing can be done in case of consanguinity. The chances of finding a full match sibling donor is 25% (chance increase with more siblings). For full match sibling donor only low resolution 6 antigen typing is just enough, however if MUD or Haplo BMT is planned high resolution 10 antigen typing of patient and donor is must. Once the donor is selected, next step is to evaluate the patient and donor for fitness which includes organ function (heart, lung, kidney, liver, etc) and infectious disease markers. Once both patient and donors are found fit, patient is admitted and informed consent will be signed by the patient or legal representative (in case of minor) and central line will be put (Hickman line, Power PICC line). These central lines are very important part of the BMT treatment process as lot IV medications, frequent blood samplings, blood and stem cell infusions will be needed.
Discharge and OPD follow up
After engraftment patients are discharged and advised to follow in OPD every week initially and then less frequently. During OPD follow up routine blood tests are done and the patients are being watched for developing any infection, GVHD or other transplant related complications. Early detection of these complications and timely intervention is the key to long term successful outcome of transplants. During early transplant phase good diet is important and so is the follow up advice, taking medicines regularly and informing each and every detail of health to the transplant team. It usually takes few months to regain the strength and getting back to normal routine, but this can only be achieved only if all the instructions are followed.
GVHD (Graft Versus Host Disease) is the reactionary attack on normal cells of recipient by the donor’s immune cells. It is two types:-
Acute GVHD
It usually occurs in the initial days after transplant and affects skin, gut and liver and depending on the symptoms it can be graded. Severe forms can be life threatening and timely treatment and intervention can improve the outcome.
Chronic GVHD
It usually occurs during the later days after transplant and can affect any organ from head to toe and the usual manifestations are that of autoimmune disease.
Mild GVHD is good in case of malignant diseases as GVL is not seen but GVHD is seen, so it is believed that if GVHD is there so will the GVL also be happening. But timely intervention is needed in case of mild GVHD transforming into severe form. But in case of non-malignant diseases, no GVHD is acceptable, that is why in these diseases immunosuppressive medication is given for prolonged period.
Every single patient is different and the full recovery period can be prolonged in some patient so it is crucial to follow the instructions and regular visits as prescribed by the transplant team.
Importance of caregiver
A caregiver is the person who will be present throughout the transplant phase starting from preparation for BMT, stay in BMT unit and post transplant follow up. The caregiver can be a person from family or friend. Emotional support is very important part of the BMT process and they need to understand clearly and carefully, all the instructions and should contact the transplant team in any need. These are important things which caregiver should take care of :-
- Giving medicines correctly at scheduled time
- Watch for soiling of central line dressing and get it changed if needed
- Taking the patient to hospital for scheduled appointments and in case of emergency
- Taking good care of cleanliness of the home and protecting from visitors and to get infections.
- Preparing and providing safe food to the patient.

Providing care to BMT patient is a full-time job and lot of things need to be compromised like your work, personal hobbies and choices, but we all know that the outcome of this effort is fruitful.
When it comes to BMT of a child the role of parents as caregiver is very vital and the whole family should take responsibility because the one person (mostly mother) is involved in the medical and emotional care, but other responsibilities has to be taken care by other member of the family. For parents whose child is planned for BMT, these are some things which can be done to encourage:-
- Talking to the child and listening to their feelings.
- They can be told about some stories and examples, and how the parents handled the situation in difficult times. One example we want to site, “one patient was advised to shave off her hair and she was accompanied by her mother-in-law, so she also had her hairs shaved off to show affection to her patient – this was really commendable.”
- Creative ways can be used to express feelings like drawing pictures, writing a story, acting out a play or singing.
- Giving comfort to the child by holding the child, hugging, back thump, etc.
- Express affection and encouragement and saying words like “I love you,” “I am proud of you” and “I support you.”
What are the questions a patient should ask the transplant team ?
- What are other treatment options?
- Why BMT is being recommended for me?
-
What is the goal of this treatment?
• To control symptoms?
• To have a long-term remission—if so, for how long?
• To cure my disease?
- How many patients have you treated who have the same disease?
- What are the chances that this treatment will get rid of the disease? For how long?
- What are the chances that I could get rid of the disease without this treatment?
- What can be done to lower the side effects?
- Is it possible to continue work or school during treatment?
- How will be my quality of life immediately after BMT and in long term?
- How long do I need to continue medication?
- How will we know whether the treatment is working?
- What other choices do we have if the treatment does not work?
- Do you know of any clinical trials that might be appropriate for me?
-
What are the possible risks and side effects of the treatment?
• First few months?
• First year?
• Long term?
If transplant is recommended then what questions you should ask?
- When should I have a transplant?
- What are the risks of waiting or trying other treatments first?
- What will be the duration of stay in BMT unit and near the hospital after discharge?
- What can I do to take care of myself and get better after transplant?
- Do I need a caregiver throughout the process?
- What does a caregiver do while I’m in the hospital and at home?
- Which family members will you test as possible donors?
- If a family member is chosen as a donor, what would he or she have to do?
- If there is no full matched donor available in the family what other options do I have (Haplo or MUD)?
- Is a haploidentical (half-matched) transplant an option for me?
- Is a reduced-intensity transplant an option?
